Introduction: Next-generation sequencing (NGS) has redefined the genetic landscape of acute myeloid leukemia (AML) and has prognostic and, potentially, therapeutic implications in AML.Advances in the biological understanding of AML pathogenesis have led to the approval of new targeted agents that increase the therapeutic options for the treatment of AML. Despite these approvals, induction chemotherapy is still widely used for the treatment of patients newly diagnosed with AML. Unfavorable risk cytogeneticand secondary AML have been associated with low responses to induction chemotherapy. In the current study, we investigated the predictive role of molecular abnormalities detected with NGS related to responses to induction chemotherapy in newly diagnosed AML patients.
Methods:We used the Medical Archival Retrieval System to identify newly diagnosed AML patients who had NGS analysis performed at our institution.. Patients treated with induction chemotherapy at AML diagnosis were included in the analysis. Response to therapy was evaluated two weeks after therapy was initiated and at count recovery. The difference in distribution of each mutation between the patients who responded to chemotherapy after one or two courses of induction chemotherapy and non-responders was analyzed using Fisher's exact test and the Cochran-Armitage Trend test. Findings with an expected false discovery rate ≤ 10% were reported as positive. The study was approved by the University of Pittsburgh IRB committee.
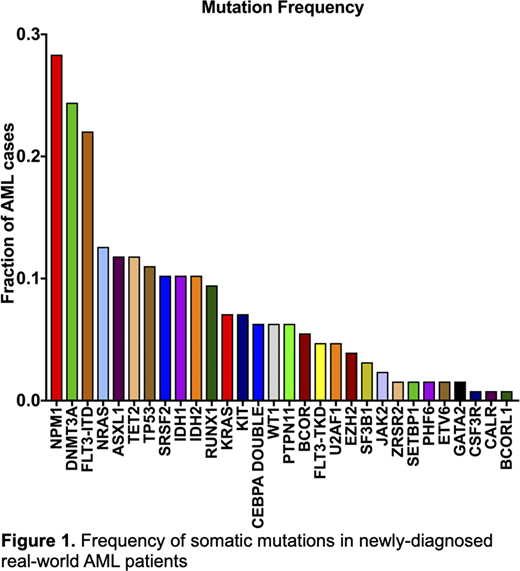
Results: One hundred twenty-seven newly diagnosed AML patients (median age 61 years, interquartile range 51-68 years) were treated with induction chemotherapy. Sixteen patients (13%) had favorable risk cytogenetics, 73 patients (58%) had intermediate risk cytogenetics, and 36 patients (29%) had unfavorable risk cytogenetics. The most common molecular event was an NPM1 (28%) mutation followed by DNMT3A (25%), FLT3-ITD (22%), NRAS (13%), ASXL1 (12%), TET2 (12%), and TP53 (11%) as shown in Figure 1. Eighty-five of 127 patients (67%) achieved CR after one course of chemotherapy with idarubicin and cytarabine (7+3) and 17 patients (13%) responded after a second course with mitoxantrone and etoposide.
Twenty-five patients (20%) did not respond to one or two courses of induction chemotherapy. From the 102 patients that responded, measurable residual disease (MRD) data were available in 59 (58%) patients. 29% patients were MRD positive and 71% patients were MRD negative. Secondary AML and poor cytogenetics were associated with poor response.
Among the 17 genes with at least 5% prevalence, only TP53 mutations were associated with worse response. TP53 mutations increased monotonically with worse outcomes; TP53 mutations were present in only 2% of those responding to one course of chemotherapy, in 18% responding to two courses, and in 38% with no response to either course (p < 0.0001). Ninety-three percent of patients (13 of 14 patients) with TP53 mutations had poor cytogenetics. After induction chemotherapy, 21% of patients with TP53 mutations achieved CR and 14% achieved morphologic leukemia-free state (MLFS); 2 patients achieved CR after one course and, after the second course, 1 patient achieved CR and 2 patients MLFS. From the 5 patients that responded, 4 had available MRD data; 2 patients were MRD positive and 2 patients were MRD negative.
NPM1 mutations were associated with higher response rates to induction chemotherapy (p =0.002). Ninety-four percent of patients (32 of 34 patients) with NPM1 mutations had intermediate cytogenetics. After induction chemotherapy, 92% of patients with NPM1 mutations achieved CR and 3% achieved MLFS; 32 patients (89%) achieved CR after one course. Two patients received a second course; one patient achieved CR and one MLFS. From the 34 patients that responded, 20 patients had available MRD data; 9 patients were MRD positive and 11 patients were MRD negative.
Conclusion: Among 17 gene mutations detected using NSG at AML diagnosis, only TP53 and NPMI mutations were associated with responses to induction chemotherapy. Patients with TP53 mutations at AML diagnosis were associated with lower response rates to induction chemotherapy, whereas NPM1 mutations were associated with improved response.
Raptis:INTEGRA: Consultancy, Other: TRAVEL, ACCOMMODATIONS, EXPENSES; UPMC: Current Employment. Hou:Genentech: Consultancy, Other: PI; AstraZeneca: Membership on an entity's Board of Directors or advisory committees, Research Funding; Verastem: Membership on an entity's Board of Directors or advisory committees; AbbVie: Consultancy, Other: PI. Dorritie:Kite-Gilead: Research Funding; Juno Therapeutics: Research Funding. Sehgal:TP Therapeutics: Research Funding; Prothena: Research Funding; Gilead Sciences: Research Funding; Merck: Research Funding; Bristol-Myers Squibb: Research Funding; Juno Therapeutics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal